Dive Brief:
- House Republicans on Sunday unveiled specifics of their plan to cut Medicaid that include more moderate reforms, but would still result in millions of Americans losing health insurance coverage.
- The House Energy and Commerce Committee — which was tasked with finding $880 billion in savings to help fund an extension of President Donald Trump’s first-term tax cuts — is proposing work requirements linking Medicaid eligibility to at least 80 hours of work, education or volunteering per month, more stringent eligibility verification requirements and freezing a financing mechanism that critics say allow states to inflate federal Medicaid funding.
- Specifics of the plan could change, as the committee is slated to consider the bill on Tuesday. But as it currently stands, the legislation would cause at least 8.6 million to lose health insurance by 2034, according to a preliminary analysis by the Congressional Budget Office.
Dive Insight:
GOP leadership has been scrambling to get its caucus to agree on healthcare cuts to help fund Trump’s “big, beautiful bill” including the president’s various tax and policy priorities.
The effort has been complicated by a tricky political calculus, given Medicaid, which along with its sister program for children covers some 80 million Americans, is deeply popular among voters — including in Republican districts.
But E&C appears to have coalesced around a plan as Republicans attempt to make a Memorial Day deadline to pass the bill, proposing new work and eligibility requirements they say will save the government money and improve program integrity.
Final legislation could look significantly different after a series of markups and public hearings on its sections this week. But at this early stage, Republican policymakers appear to have nixed more drastic Medicaid reductions that were on the table, like slashing minimum federal payments to states or capping federal spending per Medicaid enrollee.
As such, the bill text is likely a relief for providers that accept the safety-net insurance and for health insurers like Centene, Elevance and UnitedHealth that bring in significant revenue from Medicaid contracts with states.
Still, E&C’s slice of the legislation will have seismic effects for states that administer Medicaid, the providers they pay and the beneficiaries they serve, according to patient advocates and top Democrats.
“This is not trimming fat from around the edges, it’s cutting to the bone,” E&C Ranking Member Frank Pallone, D-N.J., said in a statement Sunday. “In no uncertain terms, millions of Americans will lose their health care coverage, hospitals will close, seniors will not be able to access the care they need, and premiums will rise for millions of people if this bill passes.”
One of the most significant proposed reforms is the creation of new “community engagement” requirements mandating that able-bodied Medicaid beneficiaries without dependents report at least 80 hours of work, education or volunteering each month.
That’s the same threshold as a work requirement briefly enacted in Arkansas during the first Trump administration before the it was halted by the courts. Despite the policy’s short tenure, nearly a quarter of the people subject to the work requirement lost coverage, mostly because didn’t know about the requirements or because of difficulties recording their eligibility with the state.
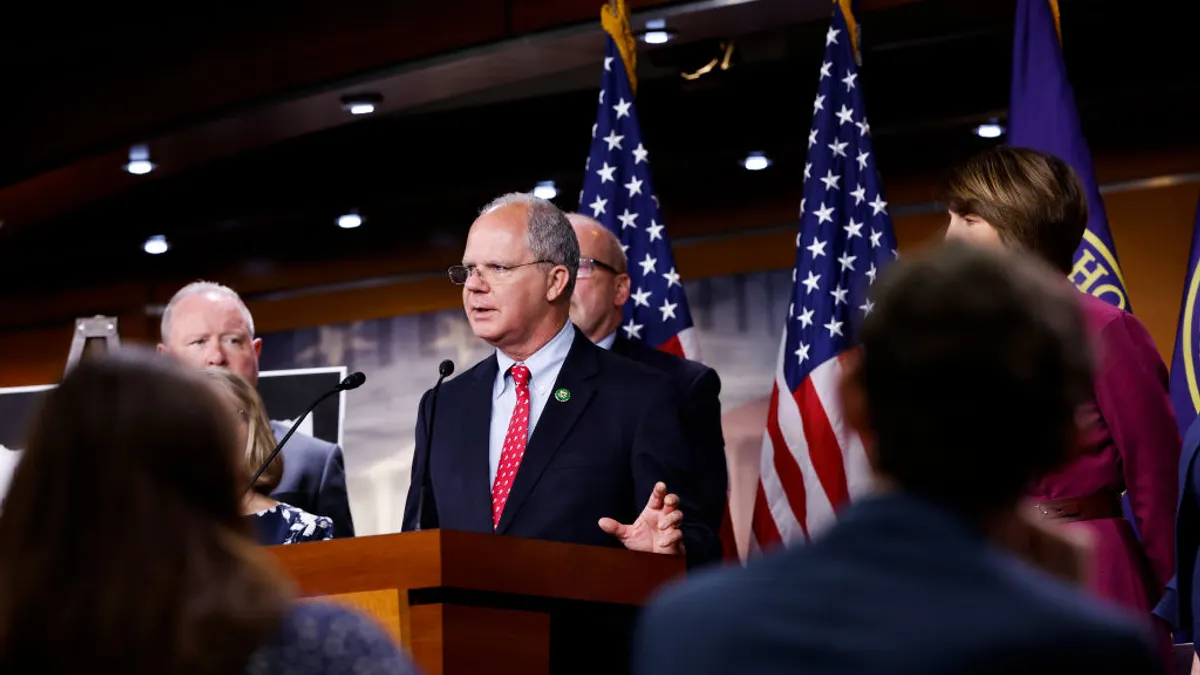
E&C Chair Brett Guthrie, R-Ky., said the bill “preserves and strengthens Medicaid for children, mothers, people with disabilities and the elderly” by cutting resources directed at “capable but unemployed adults” in an op-ed published in the Wall Street Journal on Sunday.
“Washington can’t afford to undermine the program further by subsidizing capable adults who choose not to work,” Guthrie said.
Republicans’ argument that they’re refocusing Medicaid to serve the most needy Americans by preventing freeloading is complicated by research showing most adults on Medicaid are already employed or meet exemptions from work requirements.
E&C’s bill would also let states check income and residency of beneficiaries more often — every six months rather than once a year — and allow them to cut coverage for people who don’t respond quickly.
Like work requirements, stricter eligibility verification policies have been shown to frequently remove people from coverage not because they’re ineligible but because they don’t have the time or resources to comply.
The bill would also freeze provider tax arrangements through which states, by taxing healthcare providers, can boost their Medicaid spending and receive higher reimbursement from Washington as a result. The arrangements are legal and broadly supported by providers, as they result in higher Medicaid payments, but have been slammed by critics as sneaky accounting maneuvers that allow states to benefit at the detriment of the federal taxpayer.
E&C’s legislation would also require Medicaid beneficiaries above the federal poverty line to pay higher co-payments for doctor’s visits.
Medicaid generally requires no or very low cost-sharing for its members, so the additional fee, of up to $35 for many medical services, may put treatment out of reach for some low-income Americans.
E&C is also proposing to cut federal funding for states that allow immigrants without proof of citizenship to be on Medicaid. The policy, if enacted, would affect a handful of Democrat-run states like California and New York.
The legislation, which runs for hundreds of pages, includes smaller changes like banning pharmacy benefit managers from spread pricing in Medicaid; forbidding Medicaid from covering gender-affirming healthcare for transgender individuals; and stopping Medicaid from funding providers that offer abortion care.
It would also tweak the exchanges set up by the Affordable Care Act by tightening enrollment periods and eligibility verification for subsidies and restricting automatic renewals — policies proposed by the Trump administration in a controversial rule earlier this year.
The bill, which would also roll back a number of Biden-era green energy programs, would reduce the deficit by $912 billion over the next decade, according to the preliminary CBO analysis.
The large majority of those savings — $715 billion — would be reached through the cuts to Medicaid and the Affordable Care Act.
E&C’s proposals are not as bad as some in the healthcare industry feared. For example, the provider tax reform effectively caps the state payments at the rate that Medicare pays providers instead of eliminating the arrangements entirely, which is a win for hospitals, TD Cowen analyst Ryan Langston wrote in a note on Monday.
Still, hospital groups decried the bill.
“The consequences of these cuts extend far beyond the millions of Medicaid patients impacted directly; they threaten health access for entire communities across the country,” Chip Kahn, the president and CEO of for-profit hospital lobby the Federation of American Hospitals, said in a statement Monday morning. “Congressional Republicans and President Trump rightly pledged to protect Medicaid benefits and coverage — this bill fails that test. It is imperative Republicans go back to the drawing board.”