CVS plans to launch a first-of-its-kind healthcare engagement platform, banking that perennial gripes about poor access and navigation will incentivize both consumers and rival companies to sign on.
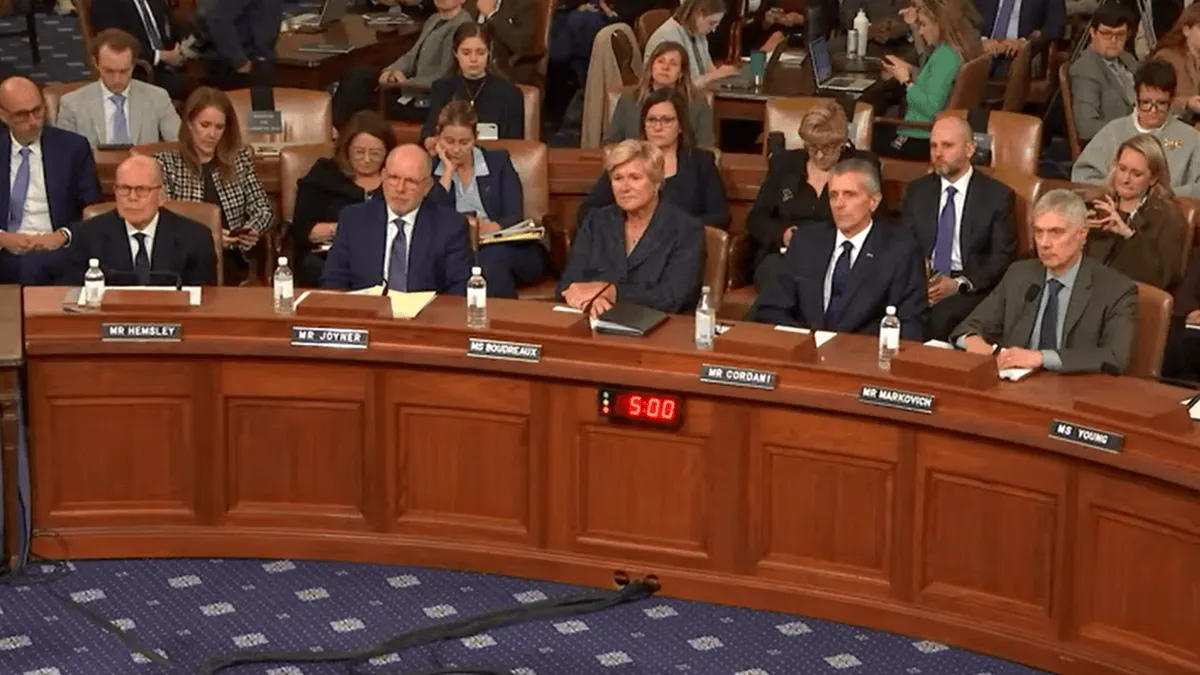
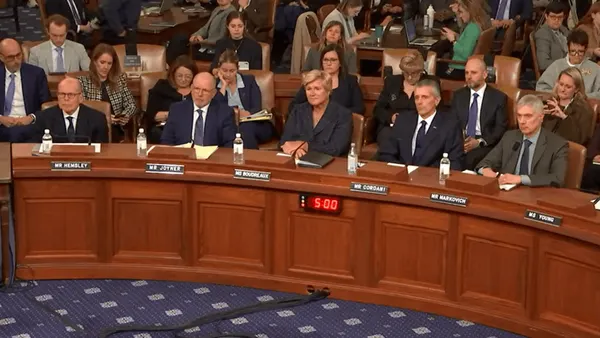
The platform will include data and services offered by CVS’ different health businesses — and those of participating industry partners. The goal is to create an integrated healthcare experience for consumers, hopefully enhancing their experience with the industry, lowering costs and improving outcomes, CVS executives said Tuesday during the healthcare giant’s investor day in Hartford, Connecticut.
CVS is also banking that the platform will also be a source of revenue by driving consumers to CVS products and services they might not know about otherwise.
CVS did not respond to questions about how much it’s spending to build the platform or how much revenue the company expects the platform to generate. The platform’s eventual value depends on if CVS is able to convince its peers in the insurance and pharmacy sectors to integrate their own data and products — not a sure bet in today’s hyper-competitive healthcare landscape.
Yet the app should help drive growth, according to one analyst.
“We look forward to hearing more but see the totality of the CVS enterprise as ripe for building out a platform like this,” Leerink analyst Michael Cherny wrote in a Tuesday note on the company’s investor day.
The engagement play
Improving customer engagement is a white whale for the healthcare sector at a time when roughly one-third of Americans don’t even have a primary care provider. Physician shortages, high healthcare prices, and confusing and complex processes have made it difficult for the average American to access healthcare, with high percentages of consumers reporting delaying or eschewing care altogether due to such factors.
The healthcare sector was laser-focused on becoming more consumer-centric prior to the COVID-19 pandemic, spurring hospitals and insurers to invest more heavily in initiatives to improve consumer engagement and experience. Though such initiatives have yielded few concrete improvements systemwide, healthcare executives say they remain a high priority. And consumerism’s importance is still evident in rising direct-to-consumer initiatives — especially in the pharmacy space.
Now, CVS is hoping that its new “engagement as a service” platform can further improve Americans’ experiences with the healthcare system, driving more revenue to its businesses along the way.
“Strong consumer engagement — a lot of companies have stood up here and said that they’re going to do that. It still remains elusive,” said Prem Shah, CVS’ executive vice president and group president, during the investor day. “Our industry has chased engagement but no one has yet caught it.”
Executives said that CVS will be able to succeed due to the company’s broad consumer reach across its Aetna health insurance, pharmacy benefit manager Caremark and retail pharmacy businesses.
Of CVS’ 185 million consumers, roughly 62 million engage with the company digitally. Twenty-one million have given CVS permission to reach them in real-time through push messaging, according to Tilak Mandadi, CVS’ chief experience and technology officer.
Creating an “everything app” combining multiple services into one platform is an idea CVS has been toying with for years. The company has taken steps by building out its CVS Health app, which now includes health benefits, pharmacy benefits, prescriptions and other data pulled from CVS’ own businesses.
But the new open engagement platform will go notably further. The platform will include a comprehensive profile for each consumer by pulling data from electronic health records, pharmacy claims, and home health and wearable devices.
It will be able to help consumers find new doctors, schedule visits and tests, and manage claims and appeals. It can suggest relevant resources and actions consumers should take to better their health or finances, like the availability of a cheaper alternative for a drug they’re taking, according to CVS.
Executives said that the platform is being built with artificial intelligence at its core, and will include an agentic AI chatbot to help consumers navigate coverage and care decisions.

But the largest thing that will set CVS’ platform apart from the some-250,000 digital health apps available in the U.S. is its potential integration with other healthcare companies.
Betting on industry buy-in
When CVS employees were creating the platform, they realized that people want integration across all healthcare entities, not just one, according to Mandadi.
CVS had already done most of the work necessary to include outside companies in the platform, so figured it could be offered up to the industry as a service, the executive said.
It’s unclear whether said companies — especially the largest conglomerates like UnitedHealth — will step onboard a platform controlled by one of their competitors, much less share their data.
Interoperability, or the free exchange of information, is a huge problem in the healthcare space. Despite regulatory efforts, patients’ data is generally siloed between different companies, making it difficult to get a comprehensive view of their health journey. There’s a business incentive for hospitals and insurers to keep data close, which makes it more difficult for patients to get health services elsewhere or switch plans, experts say — one potential roadblock for broad industry buy-in to CVS’ new platform.
Mandadi acknowledged that outside companies may be wary. But the engagement platform will help participants, he argued.
For example, pharmacies could become better at managing prescriptions and drug adherence, while insurers will be able to spur behavior change in their members. Also, participating companies will be able to create new and more personalized products from the data insights generated from the platform, Mandadi said.
“These and many other value drivers we feel are going to compel a lot of partners in the industry to participate in the platform,” Mandadi said. “Some of them probably don’t want to. But it doesn’t matter. We are very confident we’ll become a destination of choice and the consumers are going to enforce it. ‘You need to be part of this platform’ — that’s going to come from the consumers.”
CVS did not respond to questions about external interest in the platform. But CVS is having “serious” conversations with several partners that it thinks will be integrated with the platform upon its launch next year, Mandadi said.
CVS did not answer questions about the financial arrangements between CVS and companies participating in the platform, including whether they will pay CVS for access or for any new business they generate from the app.
The Rhode Island-based healthcare giant is trying to create a new growth lever for its businesses during a turnaround period. It’s been a difficult few years for CVS, as unexpectedly high medical costs have slammed its insurance arm and reimbursement troubles have dogged its legacy pharmacy business.
CVS has attempted to right the ship by reshuffling its executive bench, exiting unprofitable insurance markets and pivoting to new pharmacy reimbursement models. Those efforts have yielded some success this year. CVS has increased its 2025 earnings guidance each of the last four quarters, and again in advance of Tuesday’s investor day.