It’s an exciting time to work in care management.
My team and I are using two new powerful resources that are increasing our effectiveness while simultaneously improving the quality and cost of care for chronically-ill health plan members:
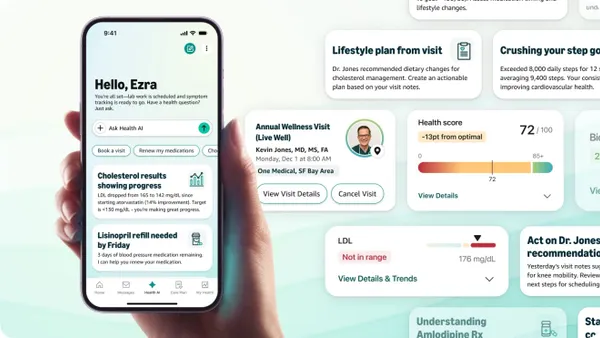
- Our use of Geneia’s @HomeSM integrated remote patient monitoring program means care managers are able to easily and effectively incorporate timely biometric data into existing case and disease management programs and use these measurements to guide earlier interventions and prevent unnecessary emergency department visits and hospitalizations.
- Our use of analytics enables us to select the health plan members most likely to participate in and benefit from remote patient monitoring.
Our approach is working and the results are compelling. Just as importantly, your health plan can achieve the same results.
Care Management: Gratifying But Demanding Work
Truth be told, I’ve always enjoyed working in care management. As care managers, my staff and I work directly with health plan members who are in the midst of a chronic or acute illness. That means we have the opportunity to positively impact their lives – and very likely their loved ones too – during an extraordinarily challenging time. It’s gratifying work, but at the same time, quite demanding.
Care managers are charged with creating an individualized and comprehensive care plan to address the complex and varied needs of chronically-ill members. The plan must effectively engage and coordinate care among the member, physicians and care team, health plan, and in many cases, the member’s loved ones and caregivers, and must do so within a budget. Typically, case managers do this important work on behalf of 60-100 members at a time; disease managers oversee 150-300 members.
That’s why I’m so enthusiastic about the power of analytics coupled with integrated remote patient monitoring to improve the lives of chronically-ill members – and the care managers charged with helping them.
Integrated Remote Patient Monitoring Works
In short, Geneia’s 12-month, scientific study comparing monitored chronically-ill health plan members to a control group demonstrated measurable success in improving the health plan’s clinical, utilization, cost and member experience outcomes. Specifically, we were able to:
- Slow disease progression: As measured by patient risk scores, the risk score of monitored members increased 29 percent compared to an increase of 58 percent for the control group.
- Reduce hospitalizations: Hospital admissions declined 76 percent for monitored members and 31 percent for the control group.
- Lower costs: Per member per month (PMPM) medical spend was 50 percent less for monitored members.
- Increase medication adherence: Pharmacy costs increased 18 percent for monitored members indicating a higher level of adherence to the care plan.
- Improve member experience: Geneia @HomeSM program participants report an overall satisfaction rate of 96 percent.
Undoubtedly, chronically-ill members benefited from remote patient monitoring, but so did our care managers. Typically, the effectiveness of care managers is judged by engagement rates, utilization in the form of inpatient admissions and readmissions and emergency department visits, costs, care plan adherence and disease progression – and all of these measures improved.
Perhaps more importantly for care managers like me, members report very high levels of satisfaction with the program and individual participants like Mr. Jack Jones tell us the improvements in their health, self-management and self-awareness mean they are once again able to enjoy social outings with friends and travel to family weddings.
To learn more about how we were able to achieve these results, read our remote patient monitoring case study.