Dive Brief:
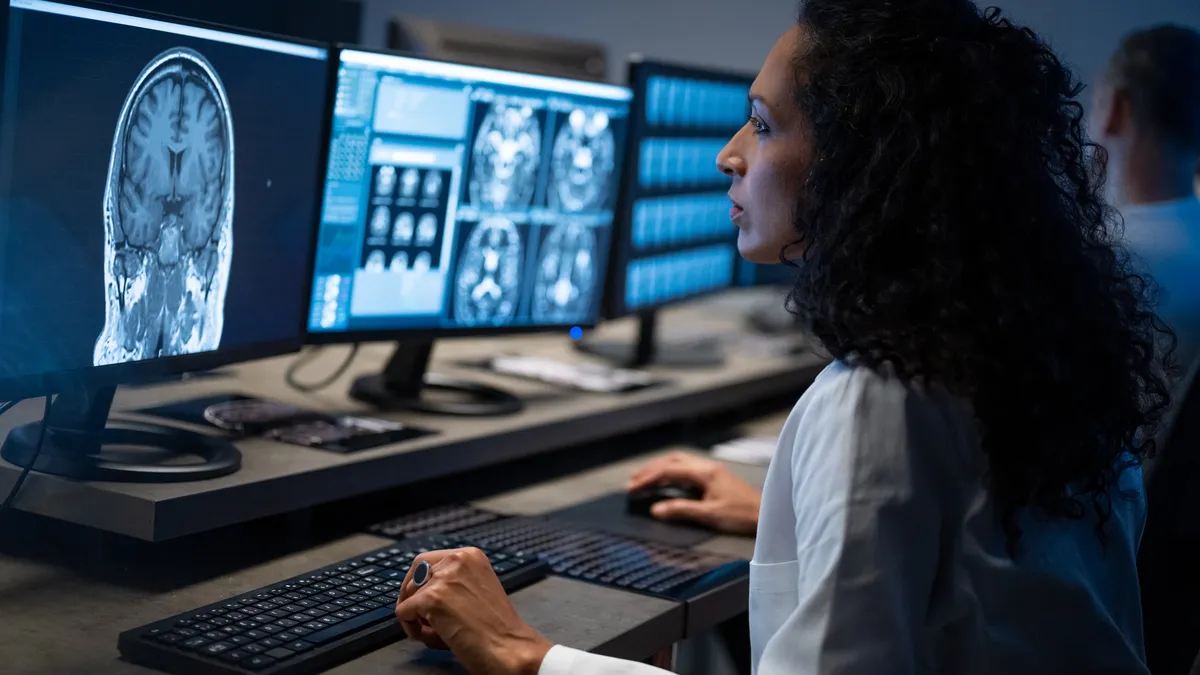
- UnitedHealthcare is raising its requirements for physicians to get paid for reviewing medical images alongside standard doctor’s appointments, according to a bulletin sent to providers last week.
- Starting in April, UnitedHealthcare’s commercial plans will require doctors like internists to submit a full written interpretation and report of radiology images in order to be reimbursed for their professional services, otherwise the insurer will consider that included in the broader payment for an evaluation and management visit.
- A physician group said the reform appeared targeted at reducing potentially improper payments for non-radiologist clinicians. UnitedHealthcare did not respond to a request for comment on the change, but it runs counter to the company’s broader efforts to pare back red tape for physicians amid widespread discontent with health insurers.
Dive Insight:
Starting April 1, when the same provider bills UnitedHealthcare for an E/M service and a global radiology code for the same patient on the same day, they won’t receive separate professional reimbursement for their services unless they attach a copy of the radiology report to their request, according to bulletin sent to providers on Jan. 1.
The heightened administration standard comes as as UnitedHealthcare and other major insurers move to strip back red tape that doctors say makes it more difficult for patients to access healthcare and for them to do their jobs. UnitedHealth, UnitedHealthcare’s parent company, has pledged to reduce the number of claims subject to preapproval and streamline other utilization management practices as the $400 billion conglomerate works to improve its relationship with lawmakers, regulators and the public writ large.
UnitedHealthcare did not respond to questions about the reason for the new requirement and whether it would increase administrative burden or lower reimbursement for providers.
Despite being targeted at radiology services, the American College of Radiology, a professional group representing U.S. radiologists, said it seemed unlikely to have a major impact on the specialists. Instead, it appears to apply to internal medicine physicians and other primary care providers that receive radiology reports like chest X-rays and review the images themselves, but may not provide the complex interpretations that would merit a professional reimbursement.
ACR is “reviewing UnitedHealthcare’s new requirement” but “initial review suggests it is directed toward non-radiologist clinicians,” a spokesperson for the group said over email. “Radiologists don’t bill E/M and are unlikely to bill for the professional component of imaging services without a complete report.”
Providers and insurers are increasingly at odds over reimbursement and what doctors view as overly onerous restrictions on care. Physicians are struggling with payment amounts they say fall well below the cost of providing care, especially from federal healthcare programs like Medicare, which outlines rate changes each year that are generally mirrored by commercial insurers.
Disputes between providers and insurers over reimbursement are increasing, as providers argue reimbursement rates have not kept pace with the escalating cost of providing care. Workforce shortages have driven up competition for labor, while inflation and President Donald Trump’s tariff policies are inflating the cost of medical supplies.
Still, payers argue they’re providing a necessary check on ever-rising healthcare costs, and say that some providers are pursuing exorbitant reimbursement increases well above the market reality — including in radiology.
UnitedHealthcare had legal or contract contests with a number of radiology practices over rates last year, including the country’s biggest radiology group Radiology Partners, Scottsdale, Arizona-based Southwest Diagnostic Imaging and Chattanooga-based Tennessee Interventional and Imaging Associates.
Correction: A previous version of this article misidentified the American College of Radiology. The error has been fixed.