The Trump administration’s top Medicare official is coming to the defense of the 2027 Medicare Advantage rate notice, after the rule sparked a wave of backlash from the health insurance sector.
The CMS proposed a flat rate update for next year, which won’t adequately cover higher spending on seniors in the privatized Medicare program, insurers say. Regulators also proposed reforms to MA risk adjustment that would restrict insurers’ ability to inflate members’ risk scores and, correspondingly, their reimbursement from the federal government.
The rule sent a shockwave down Wall Street, which had expected a much higher update from the historically pro-business Trump administration.
Publicly traded health insurers’ stocks plummeted after the rule was released in aftermarket trading Monday, and stayed down. Shares in the two largest MA carriers, UnitedHealth and Humana, were both down about 20% Tuesday afternoon, erasing tens of billions of dollars in market value.
“Much has been made about the advance notice since it was released after market close yesterday,” Medicare Director Chris Klomp said during a Paragon Health Institute event on Tuesday. “Is the administration not supportive of Medicare Advantage? Or did the market simply misread? Or is this a sign of unfriendliness or hostility to come to the market?”
None of the above, Klomp argued. The flat rate update was based on CMS actuaries’ analysis of underlying medical cost trends, and doesn’t represent any weighting one way or another by the Trump administration, he said.
Moreover, the risk adjustment changes aren’t meant to penalize the market, but to ensure the long-term stability of MA, according to Klomp.
MA has increasingly been scrutinized for driving unnecessary taxpayer spending. The federal government is set to pay $76 billion more on MA seniors than it would if those same seniors were in traditional Medicare, in part due to payer upcoding, according to congressional advisory group MedPAC.
Other research by CMS officials in the Trump administration suggest that delta is smaller. Still, risk adjustment was created to make sure plans couldn’t cherrypick healthier members, not give larger and wealthier companies with more resources a competitive advantage, Klomp argued.
“If you’re better at it than me because you have more resources than me, or are cleverer than me, or you decided to focus all of your attention on doing that really well ... that is not the point,” Klomp said.
But “make no mistake. Let me not mince words in the least. We are massively in support of Medicare Advantage,” the Medicare director said.
Klomp’s promises that the CMS is supportive of the MA program — at least a more competitive and trustworthy version — are unlikely to assuage anxious insurers that have seen their Medicare earnings crater over the past few years.
Hours before the Paragon event, UnitedHealth forecasted that its 2026 revenues would fall compared to the year prior for the first time in decades, in part due to ongoing challenges in MA.
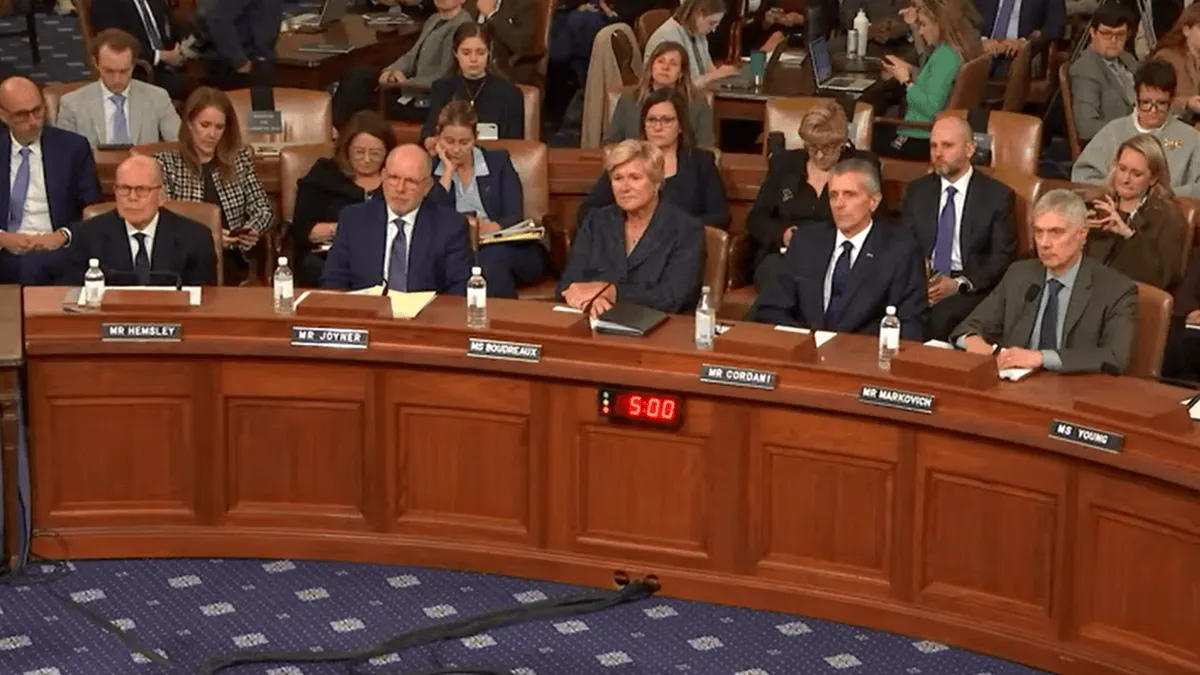
Meanwhile, insurers have emerged as a villain on Capitol Hill amid a Congress laser-focused on increasing healthcare affordability at a time of acute stress for American pocketbooks. Last week, insurance CEOs were dragged to the Hill for a marathon day of hearings in which the executives caught flak from lawmakers on both sides of the aisle, including for upcoding in MA.
President Donald Trump has said that insurers make too much money, while CMS Administrator Dr. Mehmet Oz — historically a huge supporter of MA — has acknowledged more needs to be done to curb upcoding. It’s a sharp about-face from the first Trump administration, a time when MA payers enjoyed lucrative margins in the privatized Medicare plans and relatively low oversight.
If 2027 payment rates are finalized as proposed, insurers have threatened to further cut back their MA plans, continuing the contraction that started in 2024 when rising medical costs and unfavorable regulatory changes began to hit in earnest. Plan exits, shifting premiums and lower benefits have already caused angst for U.S. seniors during the turbulent open enrollment period for MA coverage in 2026.
About 1 million fewer people will participate in the privatized Medicare program this year as a result, according to CMS estimates — shrinking MA’s share of the overall Medicare population for the first time in nearly two decades.